[retweet][facebook]
Acupuncture combined with herbal medicine is effective for the treatment of lumbar disc herniations. Beijing Timber Factory Worker’s Hospital researchers investigated the effects of warm needle acupuncture and Chinese herbal medicine on patients with lumbar disc herniations. The combined therapy produced a 69.2% total effective rate. Using warm needle acupuncture as a standalone therapy absent the use of herbal medicine produced a 50.7% total effective rate.
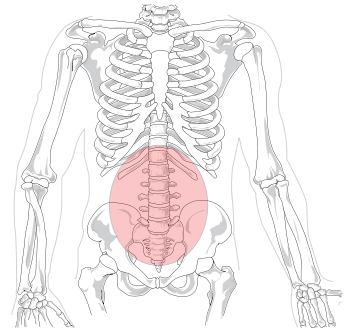 All patients included in the study suffered from lumbar disc herniations due to cold dampness. In Traditional Chinese Medicine (TCM), lumbar disc herniations are categorized into several differential diagnostic patterns including cold dampness, damp heat, qi and blood stasis, and kidney qi deficiency. The pattern investigated in this study, cold dampness, is characterized by lower back pain, tingling, numbness, range of motion impairments, a sense of heaviness in the lower back, and radiculopathy (pain, weakness, or numbness along the path of the impinged nerve). Cold dampness type herniations are chronic and are exacerbated by exposure to cold, dampness, and excess sitting, lying, or inactivity.
All patients included in the study suffered from lumbar disc herniations due to cold dampness. In Traditional Chinese Medicine (TCM), lumbar disc herniations are categorized into several differential diagnostic patterns including cold dampness, damp heat, qi and blood stasis, and kidney qi deficiency. The pattern investigated in this study, cold dampness, is characterized by lower back pain, tingling, numbness, range of motion impairments, a sense of heaviness in the lower back, and radiculopathy (pain, weakness, or numbness along the path of the impinged nerve). Cold dampness type herniations are chronic and are exacerbated by exposure to cold, dampness, and excess sitting, lying, or inactivity.
One of the most common types of lumbar disc herniation presentations is lumbar disc herniation with cold damp syndrome (Li & Wang). Common treatment methods include surgery, injections, medications, acupuncture, moxibustion, traction, and electroacupuncture (Sun, Wang & Xu). According to TCM principles, the Du (Governing Vessel), Bladder Foot-Taiyang, and Gallbladder Foot-Shaoyang channels are primarily affected by cold damp type disc herniations. The condition is often alleviated by warmth and therefore standalone moxibustion or warm needle acupuncture using moxibustion or a TDP heat lamp may be used to alleviate cold damp type disc herniations. The researchers followed standard TCM protocols and included moxibustion in their procedures.
Each acupuncture session lasted for 45 minutes. Patients received one acupuncture treatment per day for 15 consecutive days, comprising one course of care. In total, 3 courses of care were applied with a 2 day break between each course. Treatments began with patients in a prone position. Acupoints were disinfected with a 75% alcohol solution. Perpendicular insertion of filiform acupuncture needles at a high needle entry speed was used with 28 gauge acupuncture needles. The 28 gauge needle diameter is 0.35 mm and is labeled a #10 gauge in the Japanese system. This stout gauge is commonly applied in mainland China but is less common in the USA.
Manual acupuncture techniques were applied with lifting, thrusting, and rotating techniques to obtain deqi and for the purposes of applying attenuating and reinforcing methods. Once deqi was obtained at each needle, the needles were retained for the duration of the treatment session. Deqi was determined as a measure of the patient’s experience of soreness, numbness, or an electric sensation produced by the needle. Practitioner observations of needle reactions were also used to indicate the arrival of deqi. Moxibustion was added to the Huatuojiaji, BL23 (Shenshu), and BL40 (Weizhong) acupoints. Medicinal moxa pieces of approximately 2 cm were attached to the needle handles and ignited. Thick paper heat shields were placed over the skin for protection.The herbs Tao Ren and Hong Hua were added for patients diagnosed with blood stasis. Note: this herbal formula is only appropriately administered by licensed acupuncturists and is contraindicated for pregnant women. The combined therapy of acupuncture and herbs achieved a 69.2% total effective rate.
Huang et al. achieved superior positive patient outcome rates in their investigation. People’s Hospital of Han Nan District researchers (Huang et al.) achieved a 90% total effective rate for the treatment of lumbar disc herniations with acupuncture plus moxibustion. Acupuncture as a standalone therapy produced an 85% total effective rate. A significant reduction or elimination of lower back pain and radiculopathy was achieved plus motor functional improvements were confirmed with diagnostics.
Treatment was administered once per day for 6 days followed by a 1 day break from treatment. Next, an additional six days of acupuncture plus moxibustion was applied. A 90% total effective rate was achieved using acupuncture plus moxibustion. An 85% total effective rate was achieved using acupuncture as a standalone procedure.
Excerpt from:
